Physical Therapy for Knee Osteoarthritis
Knee osteoarthritis is a degenerative joint condition characterized by knee pain, stiffness, and decreased strength. Osteoarthritis generally occurs over time, slowly eroding the cartilage of the bones of the knee joint due to overuse, poor mechanics, or injury. Physical therapists can help to reduce knee osteoarthritis symptoms, slow the progression of the disease, and create a customized, comprehensive program of exercise and manual therapy to help knee osteoarthritis patients move safely and improve function, strength, and range of motion in the knee joint.
What is Knee Osteoarthritis?
Arthritis is the leading cause of joint pain in the United States. Arthritis is a chronic, progressive condition that causes inflammation, swelling, pain, and stiffness in joints. Osteoarthritis (OA) is the most common form of arthritis affecting 27 million Americans with 1 in 2 Americans developing knee osteoarthritis by age 85. Osteoarthritis of the knee is a degenerative joint disease characterized by knee pain, stiffness, and decreased strength.
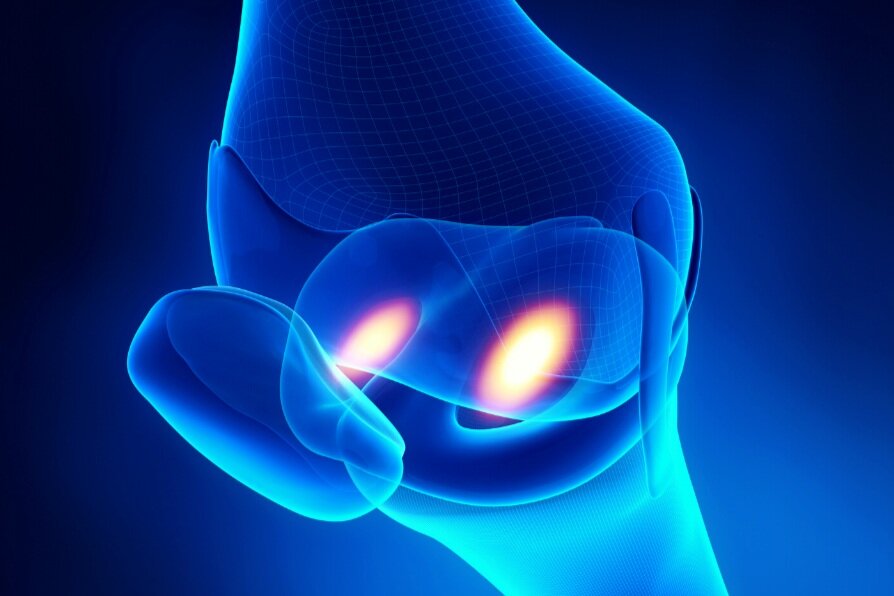
With osteoarthritis, the rubbery cartilage that coats the ends of bones at joints breaks down. Cartilage lubricates joints, distributes the force placed on the joint, and helps reduce friction when you move. As the cartilage breaks down, the bones at the knee joint can begin to rub together during movement, causing pain, swelling, and damage to the bones. Knee osteoarthritis generally occurs over time, slowly eroding the cartilage around the tibia and femur, but it can occur earlier due to trauma or an accident to that joint.
Factors that increase the risk of knee osteoarthritis include:
Age: as we age, the risk of osteoarthritis increases due to natural degeneration and aging of the cartilage and synovial fluid that lubricate joints over time.
Past injury: An injury to a specific joint, such as to the knee, can increase the risk of developing OA later in life.
Genetics: Some individuals have a more difficult time forming cartilage.
Obesity: Becoming overweight or obese places significant stress on weight-bearing joints, particularly the knees.
Occupation: Certain jobs place undue stress on the knee with repetitive squatting, bending, twisting, or prolonged kneeling, e.g. construction, childcare, landscaping, mining, or flooring specialists.
Sports: athletes who repeatedly use a specific joint in extreme ways or engage in repetitive high-impact joint loading are also at increased risk of developing OA, e.g. pitchers, linemen, ballet dancers, and runners.
Symptoms of knee osteoarthritis include:
Stiffness in the knee, especially in the morning which eases in less than 30 minutes
Stiffness in the knee after prolonged sitting or lying down
Pain during activity that is relieved by rest
Pain when you press on the knee
Cracking, creaking, crunching, or another type of joint noise in the knee
Locking or catching sensation in the knee
Increased bone growth around the joint that you may be able to feel
Difficulty engaging in daily activities: walking, squatting, climbing stairs, or getting in and out of a car
Physical Therapy for Knee Osteoarthritis
Physical therapy can help to reduce knee osteoarthritis symptoms and slow the progression of the disease. Physical therapists create a customized, comprehensive program of exercise and manual therapy to help knee osteoarthritis patients move safely and improve function, strength, and range of motion in the knee joint. Regular exercise is the cornerstone of osteoarthritis management and physical therapists are experts in prescribing the right dose and type of exercise for your condition, age, fitness level, goals, and deficits.
Studies have shown that exercise is one of the most effective treatments for knee osteoarthritis to reduce pain and improve joint motion and that exercise therapy results in better outcomes for OA patients than medication, injections, or surgery. A systematic review of 5,000 knee OA patients revealed that land-based therapeutic exercise significantly reduced pain and improved physical function and quality of life immediately following treatment. These improvements were sustained for up to 6 months after the end of formal treatment.
Another study assessed 134 individuals with knee osteoarthritis in which one group was assigned to the home exercise group only and a second group was assigned to the clinical group that received supervised exercises, individualized manual therapy, and home exercise. After 1 month, both groups showed clinically and statistically significant improvements in function and distance walked. However, the clinical group achieved twice as much functional improvement compared to those who completed unsupervised home exercises and the clinical group was less likely to take pain medication to manage their arthritis.
Physical therapy treatment for knee osteoarthritis involves:
Pain management modalities: use of ice and heat to manage arthritic pain flare-ups.
Low-impact aerobic exercise: engaging in low-impact exercises that do not put too much pressure on the knee such as swimming or a stationary bicycle to improve overall fitness and aerobic capacity.
Strengthening exercises: targeted strengthening of the muscles around the knee for increased joint stability and mobility as well as strengthening of the hip and core. Strengthening exercises can involve the use of cuff weights, resistance bands, and weight-lifting equipment.
Balance and gait training: The therapist works with the patient to maintain balance and adjust to uneven terrain, surfaces, and elevations while engaging in daily functional tasks.
Posture training: Proper posture can take the stress off arthritic joints when sitting, standing, and walking.
Manual therapy: hands-on soft tissue and joint mobilizations to increase knee joint mobility and muscle flexibility and reduce stiffness
Aquatic therapy: exercising in a warm water therapy pool allows arthritic patients to exercise with reduced pain and greater ease of movement. The warm water reduces the weight-bearing stress on the joints, decreases inflammation, and provides temporary pain relief.
Lifestyle education and changes: lifestyle changes include maintaining a healthy weight, regular movement of the knee to reduce stiffness, wearing supportive shoes, and protecting the knee when sitting (flexing the knee often and avoiding sitting for more than 30 minutes).
If you are experiencing knee arthritic pain, give our physical therapists a call to start your customized therapy program toward pain relief and improved function and mobility!