Treating Shin Splints During Soccer Season with Physical Therapy
Shin splints are a common soccer injury that involves inflammation of the tibia and surrounding muscles, which strain where they connect to the tibia and develop micro-tears, causing pain through the lower leg. Shin splints often occur early in the season during intense conditioning due to a rapid increase in the frequency and duration of exercise that places too much stress on the shin bone and muscles. Physical therapy can help soccer players manage shin splint-related pain, restore function and strength in the lower leg, and help athletes return to sport safely.
What are Shin Splints?
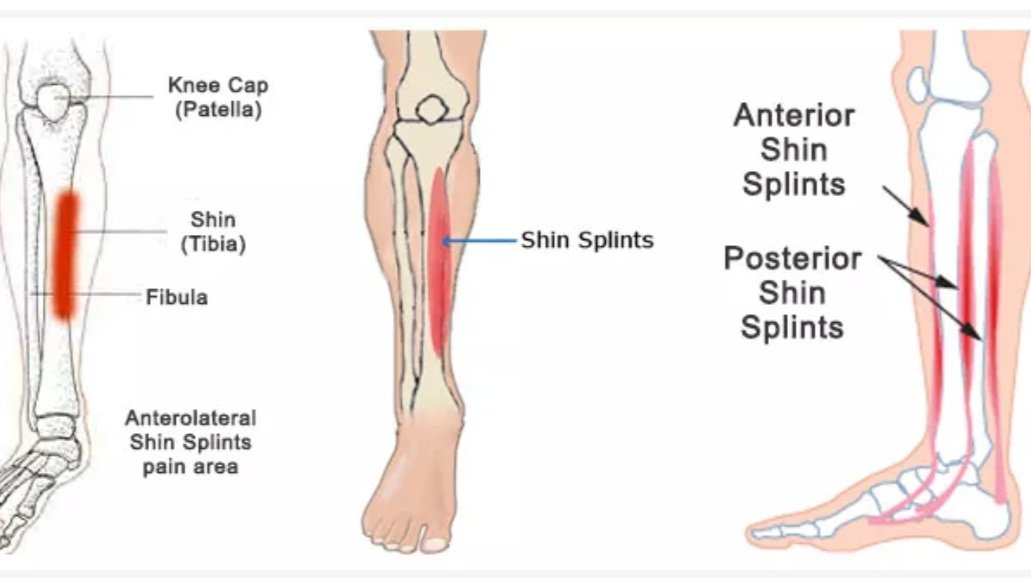
Shin splints are an inflammatory condition of the tibia and the muscles that attach to the tibia in which the bone and muscles become tender and inflamed. The muscles strain where they connect to the tibia and develop micro-tears, causing pain throughout the lower leg.
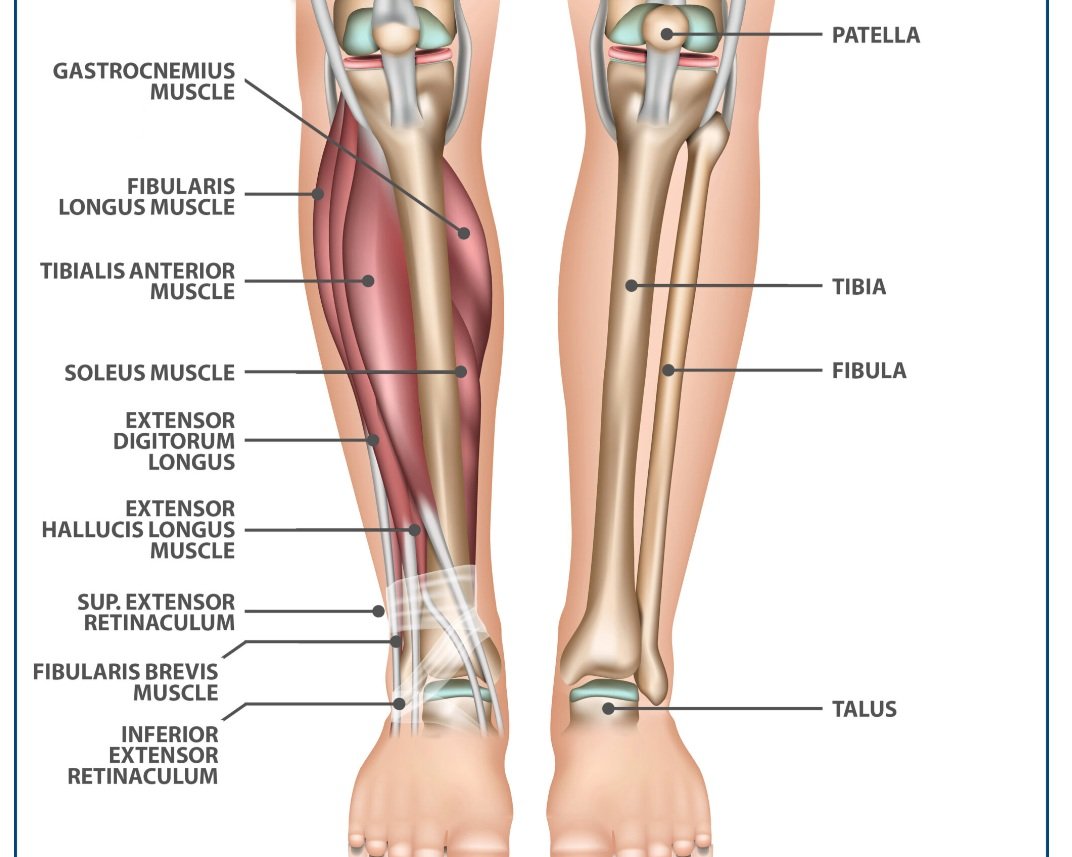
The lower leg is comprised of the tibia (shin) and fibula bones, where the muscles in the lower leg attach. Shin splints most often involve the tibialis posterior muscle, digitorum longus muscle, and the soleus muscle where they attach to the tibia bone. When these muscles become overworked and fatigued while trying to provide stability to the ankle and foot, they become inefficient at absorbing shock in the lower leg. This then places undue stress on the shin bone and the muscles, leading to pain and inflammation.
Symptoms of shin splints include a dull ache in the shin, pain on the inside of the shinbone and along the front edge of the shin where muscles attach, numbness or weakness in the feet, and pain that develops when exercising. Symptoms can show up suddenly but usually develop gradually over time.
Shin splints can lead to stress fractures if left untreated. When there is a repetitive load on the shin area without proper recovery, this contributes to an imbalance between bone formation and absorption that can result in a stress fracture to the tibia bone.
Shin Splints During Soccer Season
Shin splints are a common soccer injury due to the vigorous running and intensity of the game. It often occurs early in the season during intense conditioning or when there is a significant increase in training or high-impact kicking and jumping during the season.
Shin splints most often develop when an athlete first begins the sports season or has recently increased the duration, frequency, or intensity of their workout. Repetitive pounding and stress on the muscles, tendons, and bone tissues of the lower leg from running, jumping, and kicking can contribute to recurring trauma, pain, and inflammation that lead to shin splints.
Common causes of shin splints include:
A sudden increase in intensity and frequency of workouts or training too heavily too soon without allowing the body to gradually adapt to the workout over time
Training on an incline or doing a great deal of hill training
Past history of injuries to the foot and ankle, like ankle sprains, heel issues, plantar fasciitis, or calf strains
Overuse from training too hard without sufficient recovery
Wearing improper or worn-out footwear
Training on hard or uneven surfaces that place additional stress on the leg and shin
Incorrect soccer technique that tightens certain muscles and weakens others
Flattening of the arch of the foot when standing, walking, or running. The posterior tibialis muscle must work extra hard to control the fall of the arch of the foot and transfer the force toward the big toe of the foot, leading to overuse of the muscle and inflammation.
Abnormalities in the body such as misalignment, muscle weakness, and muscle inflexibility, e.g. changes in the range of motion of the hip which alters running kinematics and leads to excessive loading of the tibia.
Limitations in trunk, pelvis, and hip control can lead to increased loads on the tissues of the lower leg. Decreased knee flexion when weight-bearing can also contribute to shin splints.
Ankle dorsiflexion (raising toes toward the nose) stiffness leads to tightening of the tibialis posterior and digitorum longus muscles. Ankle plantarflexion (foot on the gas pedal) weakness also contributes to an increased risk of shin splints.
Incorrect biomechanics, such as altered foot, knee, and hip posture. Those who land when running more on their heel end up with more stress on the inside and outside of the shin. Weakness in the calf muscles also alters the way you move, placing undue stress on the shin.
Physical Therapy for Shin Splints
Physical therapy can help soccer players manage shin splint-related pain, restore function and strength in the lower leg, and help athletes return to sport safely. It’s key to allow for sufficient rest and refrain from aggravating activity to allow the shin and muscles to recover and reduce inflammation.
Physical therapy treatment for shin splints can include:
Pain management with ice to control swelling and reduce inflammation
Compression to promote blood flow and healing
Specific stretching of the calf muscles
Manual therapy: hands-on soft tissue and joint mobilizations to restore mobility and address restrictions in range of motion, focusing on stiffness in the foot, ankle, or calf
Targeted strengthening of the hip, core, leg, ankle, and foot to reduce pressure on the tibia and surrounding muscles with a specific focus on strengthening the calf and ankle muscles
Aerobic conditioning and cross-training to maintain fitness without placing stress on the tibia, such as swimming, cycling, or aquatic therapy exercise
Movement re-education and gait training for proper biomechanics when running
Soccer-specific agility, speed, and skill drills progressing to dynamic balance and coordination training so that the athlete prepares for the forces of high-impact activities during soccer. This can also include modified take-off and landing techniques for jumping.
Patient education on training progression and appropriate footwear for soccer to minimize the risk of developing shin splints again
Use of orthotics or shoe inserts to support the arch of the foot
Are you a soccer player suffering from shin splints? Work with a physical therapist to address shin splint pain and regain function to return to the competitive field!