Physical Therapy for Shoulder Osteoarthritis
Shoulder osteoarthritis occurs when the cartilage that lines the shoulder joint is worn or torn away, causing pain, swelling, and reduced function in the shoulder. Shoulder osteoarthritis most commonly affects those over age 50, particularly older women. Physical therapy can help those with shoulder osteoarthritis manage and decrease pain, prevent progression of the disease, and restore movement and function in the shoulder. If the osteoarthritis is severe, surgery may be recommended to restore function followed by intensive rehabilitative care.
What is Shoulder Osteoarthritis?
Shoulder osteoarthritis occurs when the cartilage that lines the shoulder joint is worn or torn away. The glenohumeral joint, where the humerus and glenoid (ball and socket of the joint) meet, and the acromioclavicular joint where the clavicle glides along the acromion, the highest point of the scapula, are more prone to the development of osteoarthritis. The prevalence of osteoarthritis increases with age, most commonly affecting those over age 50, particularly women.
Shoulder arthritis can be caused by wear and tear of the shoulder over time. Osteoarthritis of the shoulder can develop after (even years after) a shoulder joint injury or surgery from a broken bone, dislocation, or trauma. Chronic shoulder joint stress from repetitive lifting of objects overhead or throwing causes ongoing micro-trauma to the shoulder that can lead to osteoarthritis. A congenital defect in the shoulder like poor bone alignment can contribute to more shoulder dislocations and subsequent shoulder arthritis. Autoimmune diseases, like rheumatoid arthritis, and obesity can also contribute to osteoarthritis development due to the systemic inflammation throughout the body,
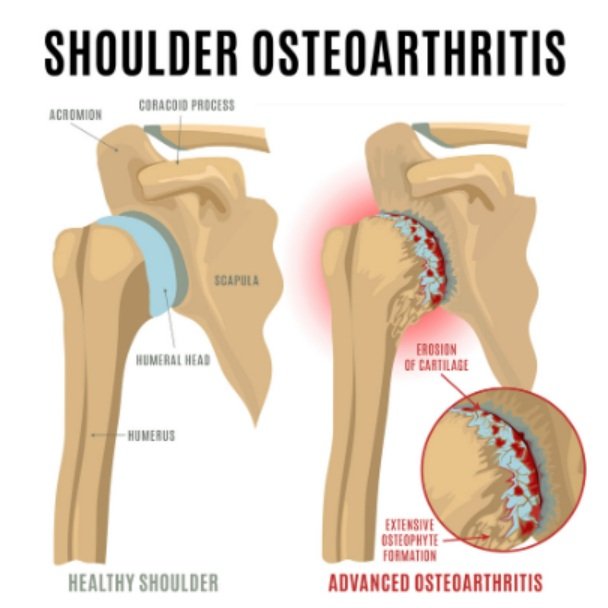
Cartilage is a strong, slippery living tissue that makes the contact between bones softer, allowing multiple rotations at the shoulder joint, helping bones glide against each other, and acting as a buffer to protect the bones from impacting one another. Cartilage is thinner at the shoulder than at the hips and knees. When cartilage begins to wear away with osteoarthritis, this negatively affects shoulder biomechanics and causes the humerus and glenoid from rubbing and grinding against each other, leading to pain and swelling. The degeneration of the cartilage develops over time through a series of stages. Initially, the cartilage begins to soften before developing cracks on the surface. During the next stage, the cartilage begins to deteriorate and flake until finally it is worn away to expose the surface of the bone.
As the cartilage deteriorates, the body can compensate by producing excess cells that form small, scalloped growths called bone spurs, which change the shoulder’s range of motion. The synovium, a delicate membrane that surrounds the shoulder joint and produces joint fluid that supplies nutrients to the joint, can also become inflamed, becoming thicker and changing in quantity and composition. These changes in the shoulder joint can also lead to changes in other soft tissues like tendons, ligaments, and bursae, which may experience excess strain and friction as the joint space between bones shrink.
Common symptoms of shoulder osteoarthritis include:
Shoulder pain and tenderness felt deeply at the back of the shoulder. Pain is often felt during the middle range of motion rather than at the extremes of the shoulder’s range of motion. Moderate or severe arthritis may cause dull aching pain or intermittent flare-ups of pain.
Stiffness in the shoulder and loss of range of motion
Catching, where a fluid movement is interrupted and accompanied by a popping or crunching sound
Muscle weakness and atrophy due to avoidance of movement due to pain and lack of use of shoulder muscles
Swelling of the surrounding soft tissues due to the friction between the bones
Physical Therapy for Shoulder Osteoarthritis
Physical therapy can help those with shoulder osteoarthritis manage and decrease pain, prevent progression of the disease, and restore movement and function in the shoulder. Shoulder arthritis patients are recommended to work first with a physical therapist to maintain function before progressing to surgery. The goal of the physical therapist is to improve the arthritis patient’s tolerance of daily activities, improve shoulder mobility, and enhance the strength of the shoulder muscles. First, the physical therapist will conduct an evaluation, assessing the effect of arthritis on your daily activities, your range of motion in the shoulder, your posture, and the strength of your rotator cuff muscles and shoulder blade before designing a customized treatment program.
Physical therapy treatment for shoulder osteoarthritis can include:
Pain management with ice and heat
Targeted strengthening of the shoulder and upper back muscles, including the rotator cuff muscles and scapular muscles.
Range of motion exercises to gradually regain full movement in the shoulder
Cardiovascular aerobic exercise for increased overall fitness
Gentle stretching of tight shoulder, back, and chest muscles
Manual therapy soft tissue and joint mobilizations to ease pain and increase shoulder mobility
Return to work and sport functional training
If shoulder osteoarthritis is severe and significantly limits function, surgery may be recommended. Post-surgery rehabilitation with a physical therapist is essential for proper healing and restoration of function and mobility in the shoulder.
There are several types of surgeries that can be performed to address shoulder osteoarthritis, including:
Total shoulder arthroplasty: Total shoulder replacement is the gold standard surgery for older patients with advanced osteoarthritis who had intact rotator cuff muscles. It involves the replacement of the glenoid with a prosthetic polyethylene cup and the replacement of the humerus with a metal ball.
Shoulder hemiarthroplasty: This surgery involves a partial replacement of the joint, replacing only the head of the humerus with a metal ball.
Reverse total shoulder surgery: This surgery is performed when the muscles of the rotator cuff have failed or are irreparable. It involves reversing the standard total replacement; the polyethylene cup is placed on the humerus and the metal ball is placed on the glenoid. This requires the deltoid muscle to provide movement in the shoulder and compensate for the damaged rotator muscles and tendons.
Shoulder osteotomy or debridement: An osteotomy involves the removal of bone spurs to reduce friction between the top of the humerus and glenoid. Debridement involves the removal of loose pieces of damaged cartilage and smoothing out existing cartilage.
Shoulder osteoarthritis can be debilitating and limit your function and mobility in the shoulder. Work with a physical therapist to manage osteoarthritic pain and regain movement in the shoulder!