Physical Therapy for Plantar Fasciitis [Infographic]
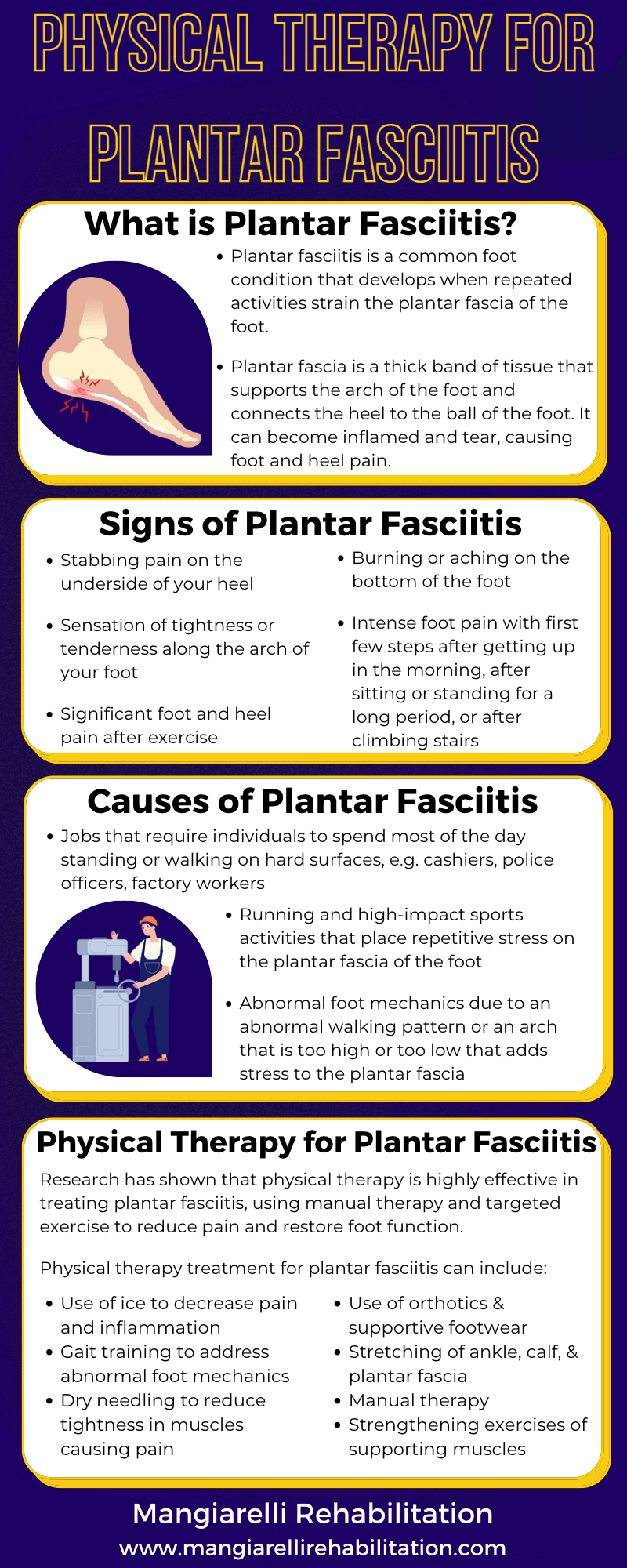
Plantar fasciitis is a common foot condition that develops when repeated activities strain the plantar fascia of the foot, which is a thick band of tissue that runs along the bottom of the foot and supports the arch of the foot. When individuals perform repetitive weight-bearing and impact-loading activities over days, months, and years, this can lead to microtears and chronic inflammation of the plantar fascia. Physical therapy is highly effective in treating plantar fasciitis, helping reduce pain, restore function and strength in the foot, improve foot mechanics, and address the root cause of the condition.
What is the Plantar Fascia?
The plantar fascia is a thick band of tissue that supports the arch of the foot and provides shock absorption when walking, running, or jumping. Plantar fascia runs along the bottom of the foot, connecting the heel to the ball of the foot and absorbing the impact of your steps when you walk. Repeated stress can irritate, inflame, or tear the plantar fascia, causing pain and limiting your movement.
What is Plantar Fasciitis?
Plantar fasciitis affects 1 in 10 Americans, impacting up to 2 million Americans each year. Plantar fasciitis is a common foot condition that develops when repeated activities strain the plantar fascia of the foot. When individuals perform repetitive weight-bearing and impact-loading activities over days, months, and years, this can lead to microtears and chronic inflammation of the plantar fascia.
Certain activities and jobs can contribute to the development of plantar fasciitis include:
Jobs that require individuals to spend most of the day standing or walking on hard surfaces, such as factory workers, police officers, restaurant workers, and cashiers, which can irritate and inflame the plantar fascia
Repetitive running and high-impact sports activities that place repetitive stress on the plantar fascia of the foot
Abnormal foot mechanics due to an abnormal walking pattern or an arch that is too high or too low can add stress to the plantar fascia by affecting the distribution of weight
Wearing shoes without appropriate cushioning, such as flip-flops, flats, or high heels
The most common sign of plantar fasciitis is significant heel pain that occurs in the morning and progresses as the day goes on or after standing for a long period of time. Symptoms of plantar fasciitis include:
Stabbing pain on the underside of the heel
Sensation of tightness or tenderness along the arch of your foot
Significant foot and heel pain after exercise
Burning or aching on the bottom of the foot
Intense foot pain with the first few steps after getting up in the morning, after sitting or standing for a long period of time, or after climbing stairs
There are several factors for plantar fasciitis that heighten the risk of developing the condition:
Being over the age of 40
Jobs, sports, or hobbies that involve prolonged standing or weight-bearing
Rapid increases in length or levels of activity, such as when starting a new running program or changing to a job that requires a lot of standing or walking
Decreased calf muscle flexibility
Dysfunction in the hip or leg muscles that affect your walking ability and change your gait, placing additional pressure on your plantar fascia
Increased body weight or obesity
Flat feet
Wearing shoes with inadequate arch support
Physical Therapy for Plantar Fasciitis
Physical therapy is highly effective in treating plantar fasciitis, helping reduce pain, restore function and strength in the foot, improve foot mechanics, and address the root cause of the condition. The physical therapist performs a thorough initial evaluation, including a review of your medical history, a pain assessment, a strength and range of motion assessment of the foot, ankle, and leg, a gait assessment and postural evaluation, and a functional movement evaluation.
Physical therapy treatment for plantar fasciitis can include:
Pain management using ice to decrease pain and inflammation
Gait training to address abnormal foot mechanics
Dry needling to reduce muscle tightness in muscles causing pain
Kinesiotaping to support the damaged plantar fascia and improve blood flow
Use of orthotics and supportive footwear to provide appropriate cushioning and support for the foot and minimize abnormal foot motion
Stretching of the ankle, calf, and plantar fascia
Manual therapy soft tissue and joint mobilizations to improve the pliability of the plantar fascia for improved weight-bearing and walking.
Targeted strengthening exercises of supporting muscles of the foot, ankle, leg, and hip muscles. The therapist may also target the gluteus medius muscle, which stabilizes the pelvis and keeps the knee from moving inward and the foot from overpronating.
Research studies have shown that physical therapy is a highly effective treatment for plantar fasciitis, using manual therapy and targeted exercise to reduce pain and restore foot function. A 2017 study showed that those who received physical therapy for their plantar fasciitis had faster recovery times; their physical therapy involved manual therapy and rehabilitative exercise. A 2019 study found that physical therapy-based stretching and strengthening exercises resulted in less pain and improved gait in those with plantar fasciitis.