Physical Therapy for PCL Injury
The posterior cruciate ligament (PCL) works together with the ACL to stabilize the knee during movement. The PCL is located near the back of the knee joint and attaches to the back of the femur and tibia behind the ACL. PCL injuries are less common than ACL injuries but can occur due to blunt trauma during a sport or car accident or extreme hyperextension of the knee. Physical therapists can help those with PCL injuries and those healing after PCL surgery manage pain and stiffness, address instability, and restore function and strength to the knee through a progressive rehabilitation program.
What is the Posterior Cruciate Ligament (PCL)?
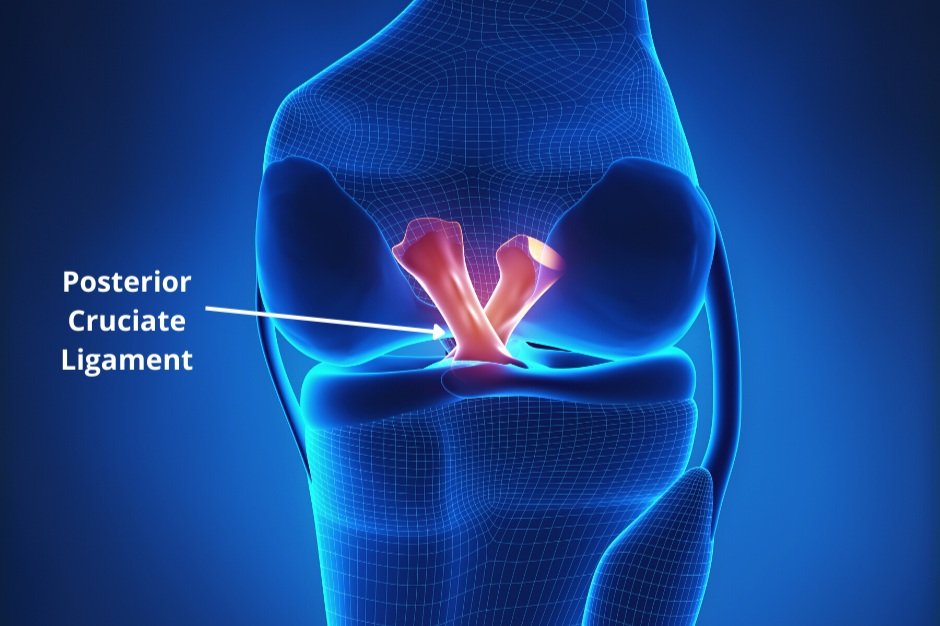
The posterior cruciate ligament (PCL) is comprised of two thick bands of tissue bundled together. One part of the ligament tightens when the knee is bent, and the other part tightens when the knee straightens. The two bundles of the PCL not only change length when the knee flexes and extends, but also change orientation from front to back and side to side, which allows the ligament to keep the shinbone from sliding too far back or slipping from side to side.
The PCL is located near the back of the knee joint and attached to the back of the femur (thighbone) and the back of the tibia (shinbone) behind the ACL. The ACL crisscrosses the PCL inside the knee joint and the ACL and PCL work together to stabilize the knee while allowing motion.
There are 20,000 PCL injuries per year in the United States. PCL injuries can occur in athletes like skiers, football and soccer players, and dancers who may leap and land on shins with bent knees. A common cause of PCL injury is when an individual or athlete lands on their shins during activity, which is a force that pushes the shinbone backward under the thighbone, stretching or tearing the PCL. PCL injury can also occur due to blunt force trauma to the knee or violent hyperextension of the knee, often in combination with other knee injuries like an ACL tear or meniscus injury. PCL injury can also occur during a car accident if the knee is bent, and the knee and shinbone hit the dashboard.
Symptoms of PCL injury include:
Sharp or dull pain inside the knee joint or back of the knee
Pain in the knee when squatting to lift a heavy load
Pain when walking over unstable surfaces or longer distances
Significant swelling and stiffness in the knee
Feeling the knee will collapse or give out
Difficulty going up or downstairs
Pain when attempting to run or jump
PCL partial tears occur more frequently than full tears. There are four grades of PCL injury that help to guide whether non-operative rehabilitation or surgery is necessary to treat the PCL injury. A Grade 1 tear is a partial ligament tear, while Grade 2 involves a partial tear and the ligament feels loose. A Grade 3 tear occurs when the ligament is completely torn and the knee is unstable, while a Grade 4 tear involves the PCL being injured and other knee ligaments being damaged.
Non-operative rehabilitation is used for Grade 1 and 2 tears, while a Grade 3 tear may require immobilization for a period of time before beginning therapy. Surgery is generally recommended if there is a full tear of the PCL, the individual has suffered multiple PCL injuries, if other knee ligaments were damaged, or if conservative treatment has failed. Surgery involves PCL reconstruction.
Physical Therapy for PCL Injury
Physical therapists can help those with PCL injuries and those healing after PCL surgery manage pain and stiffness, address instability, and restore function and strength to the knee through a progressive rehabilitation program. The physical therapist conducts a medical history and physical examination to assess the injured PCL, including performing specific stress tests on the knee and checking if any other knee ligaments or structures were damaged.
Physical therapy treatment for PCL injury includes:
Pain management and reduction of swelling with ice.
Range of motion exercises in the knee, hip, and ankle as limited mobility in the hip and ankle can place more stress on the knee.
Manual therapy: hands-on mobilizations of the knee and lower extremity to improve motion and guide the knee into a less stressful movement pattern. The therapist may perform patellar mobilization to help desensitize the knee early after injury and help restore any mobility deficits of the kneecap. This also helps for optimal bending and straightening of the knee.
Targeted progressive muscle strengthening of the quadriceps, lower extremity, and core. After a knee injury, quadriceps strengthening is critical as they play an important role in stabilizing the knee and become inhibited with knee trauma.
Functional training to learn safe, controlled movements to minimize strain on the knee and practice work and sports tasks.
Use of functional brace during and after treatment to stabilize the knee.
Return to sport testing using agility drills, step-ups, and single-leg eccentric box squats to test for readiness to return to sport.
The stages of PCL Rehabilitation for both non-operative PCL treatment and post-surgery treatment involve:
Stage 1: Protective Phase, Weeks 1-6: treatment involves pain and swelling management, use of a functional brace to stabilize the knee, knee range of motion exercises within prescribed limits, initial reactivation of the quadriceps musculature, non-weight-bearing hip activation, and manual therapy to improve knee movement. If the patient has had PCL surgery, they are to wait one week before beginning post-surgical rehabilitation.
Stage 2: Transition Phase, Weeks 6-12: treatment focuses on enhancing proprioception and strengthening the lower extremities such that the patient can perform low-impact activities without pain. The patient should achieve full knee range of motion.
Stage 3: Functional Phase, Weeks 12-16: treatment goals involve a return to activities like light jogging, core strengthening, proprioception exercises, neuromuscular control training to restore the dynamic stabilization of the knee, and the start of some agility drills.
Stage 4: Return to Sport Phase, Weeks 16-24: Treatment should progress to advanced movements and functional exercises, sport-specific agility drills, dynamic stabilization drills, and plyometrics. Return to sport testing is conducted by the physical therapist to ensure athletes can return to sport safely.
Have you recently experienced a PCL injury? Work with a physical therapist to address your pain now and regain function safely!