Physical Therapy for Foot Drop
Foot drop is a symptom of an underlying neurological, muscular, or anatomical problem involving an inability to lift the front of your foot due to an impairment in the muscle in the front of your shin, the anterior tibialis. Foot drop presents as an individual dragging the foot and toes on the ground when walking or bending the knees to lift the foot higher above ground to avoid dragging. Foot drop is commonly caused by peroneal nerve injury, lumbar radiculopathy, or neurological conditions like a stroke, Parkinson’s disease, or multiple sclerosis. Physical therapy can help address foot drop and improve functional mobility and gait pattern through a targeted therapeutic and strengthening exercise program.
What is Foot Drop?
Foot drop is a symptom of an underlying neurological, muscular, or anatomical problem involving an inability to lift the front of your foot due to an impairment in the muscle in the front of your shin, the anterior tibialis. The anterior tibialis muscle plays a large role in dorsiflexion and deceleration of the foot when walking. Damage to this muscle, whether from injury, nerve damage, or neurological or motor neuron conditions can cause the muscle to not function properly and lead to foot drop. This makes it quite challenging to walk, causing individuals to drag the foot and toes on the ground or bend their knees to lift the foot higher above ground than normal to avoid dragging, which results in an abnormal gait pattern.
Common causes of foot drop include:
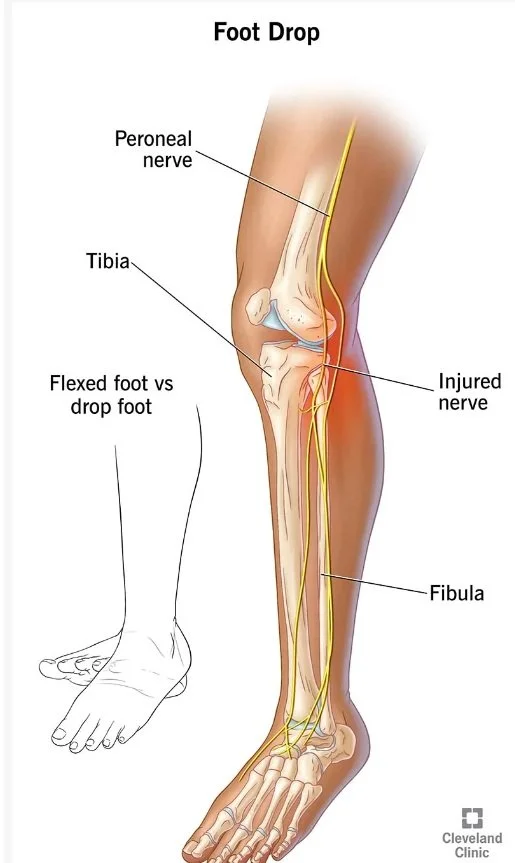
Peroneal nerve injury: The peroneal nerve is a peripheral nerve that extends down the leg, branching from the sciatic nerve, traveling down the back of the thigh, and then along the outside of the knee to the front of the lower leg. This nerve supplies movements and sensation to the lower legs, feet, and toes and is responsible for controlling the muscles that lift the foot. Peroneal nerve injury is normally caused by traumatic injury to the knee, leg, or ankle, such as an ankle fracture, fibular fracture, or knee fracture or knee dislocation. It can also result from injury to the sciatic nerve, from which the peroneal nerve branches. Individuals may be at higher risk of peroneal nerve damage if constantly sitting with legs crossed at the knee, having the leg in a cast, being on bed rest, or having conditions like rheumatoid arthritis, lupus, or diabetes.
Lumbar radiculopathy: this occurs when one of the nerve roots in the spinal column is compressed or irritated. A pinched nerve in your L5 vertebrae is a common cause of foot drop and can occur due to narrowing of the space where nerve roots exit the spine due to spinal stenosis, bone spurs, herniated discs, or lumbar spondylosis. Nerves originate in the spinal vertebrae from the spinal cord and extend down through the leg and feet, providing sensation and activation of muscles throughout the entire leg and foot.
Neurological conditions such as Multiple Sclerosis, Cerebral palsy, Parkinson’s disease, or stroke. Stroke survivors more commonly experience foot drop after a stroke due to hemiplegia, or weakness or paralysis on one side of the body.
Motor neuron conditions such as polio, spinal muscular atrophy, or ALS.
[Source: Cleveland Clinic]
Symptoms of foot drop include:
Inability to lift foot
Dragging toes or top of foot when walking
Slapping the foot on the floor with each step
Raising the leg while walking as if trying to climb stairs to avoid dragging foot (steppage gait)
Numbness in top of the toes or foot from dragging
Developing an abnormal foot drop gait to avoid foot dragging
Physical Therapy for Foot Drop
Physical therapy can help address foot drop and improve functional mobility and gait pattern through a targeted therapeutic and strengthening exercise program. Foot drop treatment depends on the underlying condition causing the foot drop and physical therapists make referrals to surgeons and specialists if the patient’s foot drop becomes permanent due to a chronic condition. However, a physical therapist can effectively address foot drop and retrain the muscles and nerves of the lower body in many cases.
The physical therapist initially completes an assessment of the individual’s function, testing foot and ankle range of motion, lower extremity muscle strength, functional mobility and outcome measures, and their balance and proprioception (awareness of the position and movement of their body).
Physical therapy for foot drop can include:
Therapeutic exercise and strengthening exercises of the muscles of the foot, ankle, and calf to help maintain muscle tone and strengthen and stretch the foot while restoring mobility to the ankle. The therapist also guides the patient through targeted stretching of the calf and foot muscles to improve mobility.
Manual therapy involves hands-on care such as soft tissue and deep friction massage, manual stretching, and joint mobilization to regain mobility and range of motion in the foot and ankle.
Functional electrical stimulation uses electrical nodes placed on the foot and lower limb to stimulate the nerves and muscles fibers with gentle electrical impulses to increase muscle tone and contractility and activate impaired muscles.
Gait training to address abnormal walking patterns and improve stability, balance, and proprioception. The therapist may use walkers, canes, or the parallel bars to safeguard the patient along with a gait belt at the start of gait training.
Neuromuscular reeducation focuses on restoring stability, retraining the lower extremity, and improving the individual’s movement technique and gait mechanics (walking, climbing stairs, stepping).
Modalities such as ice, ultrasound, and electrical muscle stimulation can help decrease pain.
Home exercise program that encompasses stretching, stabilization, and strengthening exercises of the lower extremities.
Foot drop braces and splints like the ankle-foot orthosis, which is an L-shaped brace designed to support the function of the ankle and foot by keeping them at a 90 degree angle, which helps keep the foot off the ground while walking.
Are you struggling with foot drop? Work with a physical therapist to improve your function and normalize your gait and walking mobility safely!