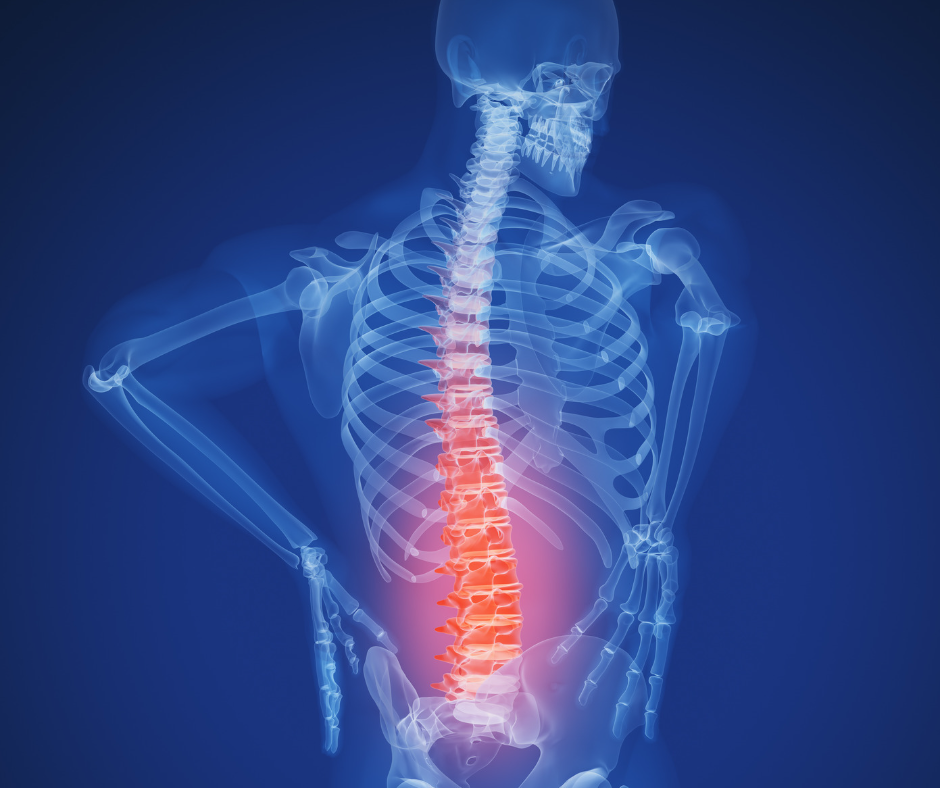
Back Pain Treatment
Back pain is one of the most common reasons individuals seek physical therapy. Twenty-five percent of Americans report experiencing back pain at some point in the last three months. Back pain can be acute (lasting less than 3 months) or become chronic (continuous pain for 12 weeks or more after initial injury). Physical therapy offers a non-surgical, non-invasive treatment option for back pain to help patients restore mobility, reduce pain, and strengthen the back, spinal, and abdominal muscles to stabilize the back and prevent future injury.
Low back pain is among the most common reasons patients come to physical therapy. Low back pain can result from poor posture and spinal alignment; a sprain or strain when lifting; a traumatic injury from a sport, fall, or car accident; or due to degenerative issues associated with age or arthritis.
Low back pain can vary from a dull ache to a burning sensation to intense, sharp pain. The pain may be located at a single point or over a broad area and cause muscle spasms or stiffness. Low back pain can lead to pain radiating through the leg (sciatica). Physical therapy treats low back pain through an exercise rehabilitation program that includes stretching, dynamic stabilization, core strengthening, low-impact aerobic exercise, postural training, and aquatic therapy. Lumbar traction and manual therapy may also be used to relieve pain.
Sciatica pain is nerve pain that radiates from the low back through the buttocks down the length of the leg due to compression of the sciatic nerve. Sciatica pain symptoms include pain in only one leg; feeling of a constant burning sensation or shooting pain down the low back through the leg; experience of numbness in the back of the leg or leg tingling/weakness; and may feel worse based on posture.
Physical therapy is the first line of treatment for sciatica pain management, relief, and treatment. Physical therapy provides symptom relief, promotes healing of the underlying cause, and improves the patient’s physical function, helping to prevent recurrences and flareups of sciatica pain. Physical therapy treatment for sciatica pain includes an aerobic conditioning program, back stretching and strengthening exercises, functional retraining and gait training, manual therapy, dry needling, aquatic therapy, and pain-relieving modalities.
Back and spinal surgery is a major surgery requiring intensive post-surgical rehabilitation to obtain the most benefit from surgery and improve function, balance, gait, mobility, and strength post-surgery. There are several types of back surgery—lumbar fusion, lumbar laminectomy, and lumbar discectomy.
After back surgery, physical therapy is essential for proper healing and to retrain the back muscles to provide stability to the spine. Physical therapy involves pain management modalities, manual therapy, gait training, and a gradual therapeutic exercise program. Exercise after spinal surgery is important in order to address fatigue, help patients return to daily activities safely, avoid re-injury, and help the body heal.
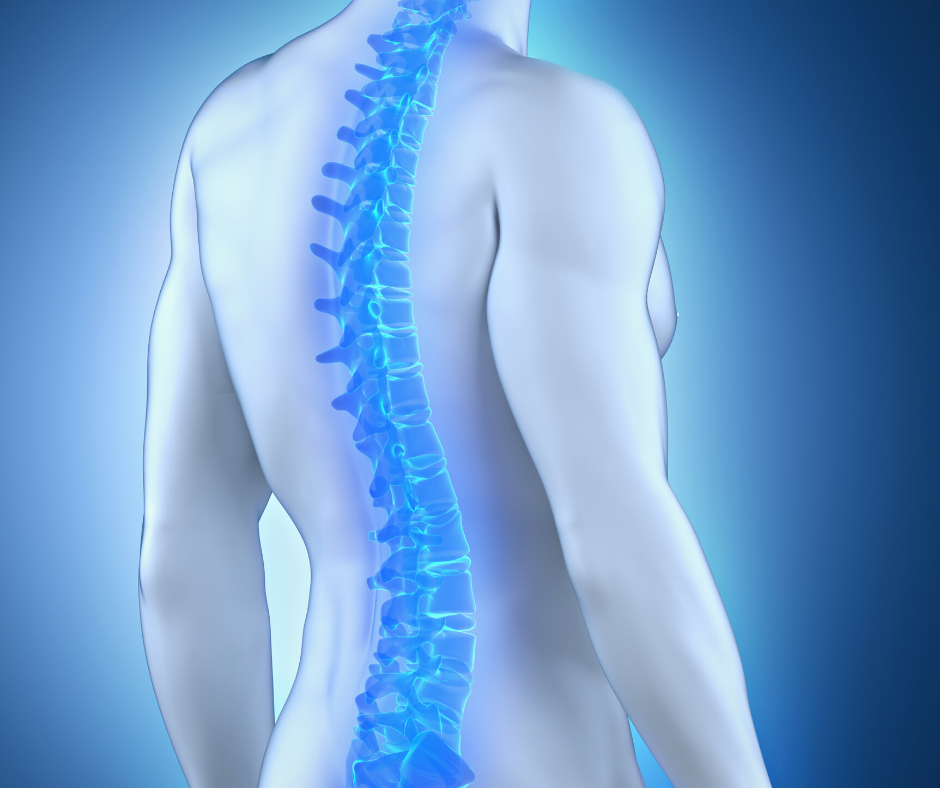
Spinal Health
The spine supports the body in all daily activities and movements with nearly every movement originating from the spine. Maintaining the strength of the upper and lower spine is critical for optimal function and to prevent injury.
The spine protects the spinal cord and associated nerve roots, provides structural support and balance to maintain an upright posture, and enables flexible motion. The spine is used by the nervous system to transmit sensory information between the brain and the rest of the body. If the spine is damaged, this interrupts the neural responses and negatively impacts the transmission of sensation throughout the body.
Physical Therapy and Spinal Health
Disorders or injuries to the spine affect nearly 80% of Americans at some point in their lives with the most common complaints being back or neck pain. Mechanical spinal pain is related to poor posture and alignment, incorrect body mechanics, lack of muscular strength around the spine, or trauma to the spine from a sport, work, or accident.
Physical therapists treat spinal disorders, reduce back and neck pain, and help to maximize spinal health, strength, and stability through spinal stabilization, manual therapy, and a therapeutic exercise program. Physical therapists specifically target the abdominal, trunk, and back muscles to build strength, endurance, balance, and control in these muscle groups to take the stress off of the spine.
A herniated disc occurs when the outer ring of the intervertebral disc of the spine is torn, allowing the gelatin-like core of the disc to leak which irritates and compresses nearby nerves. This can cause radiating pain, weakness, numbness, and loss of sensation in the back, leg, neck, and shoulder. Herniated discs are most common in the neck and back and are a common cause of low back pain.
Physical therapy is the first-line treatment for herniated discs, helping to relieve pain and restore function. Physical therapy treatment can include pain management, posture and body mechanic retraining, manual therapy, strengthening exercises; core strengthening; low-impact aerobic conditioning; aquatic therapy; and functional retraining.
Spondylolysis is a lumbar stress fracture in the pars interarticularis, the bony bridge that connects the upper and lower facet joints of the vertebrae. It is a common cause of low back pain in adolescent athletes, caused by repetitive loading, backward bending, and twisting of the lower back.
Physical therapy can successfully manage spondylolysis, helping to reduce pain, improve strength and function in the low back, and safely return athletes to sports competition using manual therapy, body mechanic instruction, and targeted strengthening of the lumbar spine, pelvis, hips, core, and buttocks.
Osteoarthritis of the Spine
Osteoarthritis is the most common type of arthritis affecting the spine, often due to age-related wear and tear and mechanical changes in the spinal discs. Spinal osteoarthritis leads to pain in the back and neck and stiffness and loss of mobility in the spine.
With osteoarthritis of the spine, you may experience pain that worsens after prolonged inactivity, swelling and tenderness around the arthritic vertebrae, loss of flexibility in the spine, and burning or tingling sensations that spread down the arm or leg due to nerve compression by spinal discs.
Physical therapy can help to reduce spinal osteoarthritis symptoms, slow the progression of the disease, and instruct patients how to safely exercise. Physical therapy treatment can include pain management, manual therapy, prescribed exercise and strength training, core strengthening, aquatic therapy, and daily activity training.
Spinal Stenosis
Spinal stenosis is a degenerative condition of the spine that involves narrowing of the openings within the vertebrae of the spinal column that results in too much pressure on the spinal cord and nerves.
Spinal stenosis can develop after the age of 50 due to the effect of aging and osteoarthritic wear and tear on the spine and spinal vertebrae. It can cause pain in the low back, sciatica pain that radiates down the length of the leg, numbness or tingling in the leg or foot, and pain that increases when you stand for a long time, walk downhill or flex backward.
Physical therapy provides effective treatment for spinal stenosis, helping patients regain function, mobility, and strength in their low back and relieving compression of the spinal nerves.